
Revolutionizing Holistic Healthcare
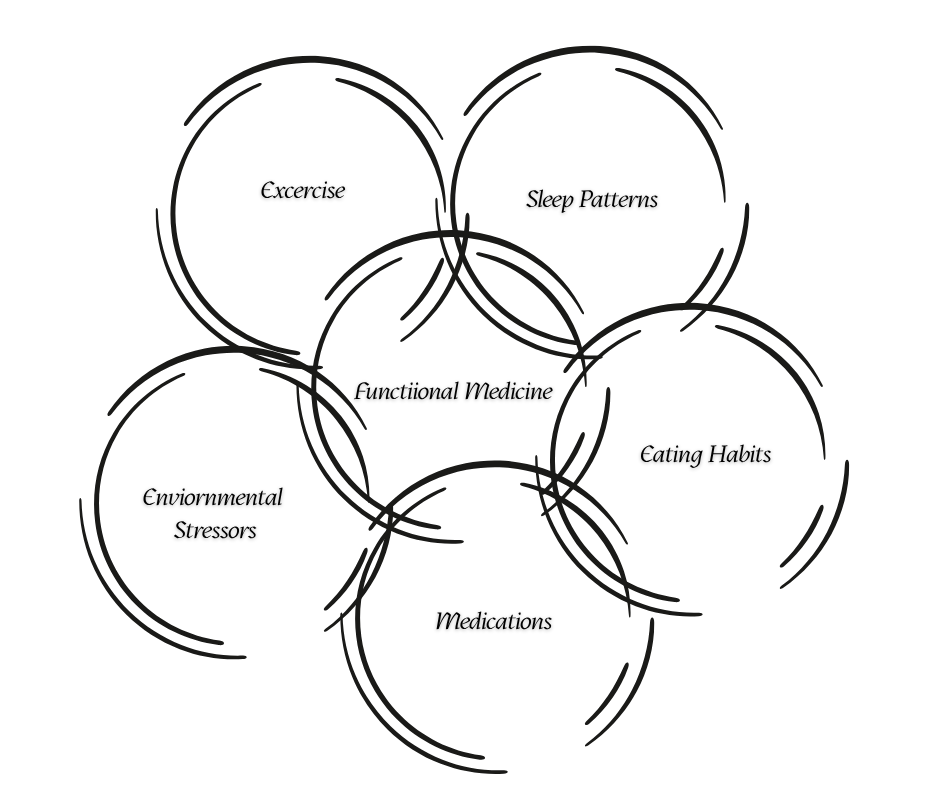
In an era where healthcare is increasingly digital, the fusion of functional medicine and telehealth stands out as a game‑changer. Functional medicine is a patient‑centered approach that focuses on identifying and addressing the root causes of disease, rather than just treating symptoms. It emphasizes personalized care, considering factors like genetics, lifestyle, biochemistry and environment to promote long‑term wellness.
Meanwhile, telehealth—delivering healthcare services remotely via video calls, apps and digital platforms—makes care easier to access without the constraints of a physical visit. The combination of these two is gaining momentum, especially post‑pandemic, as more people seek convenient holistic health solutions.
Enhanced Accessibility & Convenience
One of the most significant advantages of combining functional medicine with telehealth is the unparalleled accessibility it provides. Traditional in‑person visits often require patients to navigate traffic, take time off work, or arrange childcare — all barriers to consistent care. Telehealth largely removes these obstacles and allows patients to meet their providers from home, or even while traveling.
For patients in rural or underserved areas, this is particularly transformative. Functional medicine often involves specialists who may not be locally available; telehealth bridges that gap. Patients can access expert practitioners across states or even countries (subject to licensing) without relocating.
Because of this accessibility, no‑show rates tend to drop, continuity of care improves, and patient satisfaction increases.
Family involvement also gets simplified: With telehealth you can have loved ones join calls or share data in real‑time (such as nutrition tracking or symptom logs), which aligns nicely with the holistic, collaborative ethos of functional medicine.
Personalized, High‑Quality Care Without Compromises
Functional medicine thrives on deep, individualized assessments. Telehealth platforms enhance this by freeing the practitioner from the logistical burdens of an in‑office visit: less time spent in waiting rooms, fewer interruptions, and more focused sessions.
Technology integration fortifies this: remote monitoring tools, wearables tracking metrics like blood pressure or sleep patterns, and mobile apps for symptom logging create a data‑rich environment. For example, patients with hormone imbalances, autoimmune issues or metabolic dysfunctions can have their progress monitored digitally and treatment plans adjusted in near real‑time.
Another plus: the care team expands. With telehealth, the practitioner can more easily loop in nutritionists, health coaches, or wellness therapists—even across different geographies—so the functional medicine model (which often emphasizes an integrative, multi‑discipline approach) becomes more scalable.
Importantly, telehealth care has shown to be comparable to in‑person visits in outcome quality. A recent multi‑site study found telehealth yielded equivalent quality‑of‑life scores compared to in‑person care across a serious condition set.
Cost‑Effectiveness & Expanded Reach
Because telehealth requires less physical infrastructure (clinic space, waiting room staff, etc.), providers can often operate with lower overhead. These savings can then translate into more competitive pricing or more frequent follow‑ups for patients.
Patients save too: less travel time, no commuting, fewer logistical burdens. For people juggling busy work/life schedules, or those with mobility issues, the convenience itself is a cost‑avoidance.
Telehealth also helps widen the reach of functional medicine into underserved markets: remote regions, older adults, people with chronic conditions who struggle to make in‑person visits. This improves health equity and makes root‑cause care more broadly available.
Finally, because functional medicine emphasizes prevention and lifestyle change (rather than only acute treatment), the cost‑savings potential over time (fewer hospitalizations, less medication burden) is meaningful—though long‑term studies are still emerging.
Overcoming Challenges & Looking Ahead
No model is perfect, and this one is no exception. A few commonly cited issues:
- Technology barriers: patients with poor internet access, low digital literacy, or without privacy can struggle.
- Licensure/regulation: Providers must be licensed in the patient’s state (in the U.S.), which sometimes limits cross‑state access.
- Limitations of remote care: Some conditions absolutely require in‑person exams, imaging or procedures. Telehealth may serve best as a complement.
Looking ahead: the future is exciting. Emerging technologies like AI‑driven health analytics, advanced wearables, continuous biomarker monitoring and virtual‑reality wellness coaching are poised to deepen the tele‑functional medicine connection.
Conclusion: Embracing a Healthier Future
The benefits of functional medicine delivered via telehealth are clear: greater accessibility, personalized care, cost‑effectiveness and the ability to expand holistic wellness to more people. By addressing root causes remotely, this model empowers patients to take charge of their health without the traditional barriers of bricks‑and‑mortar visits.
If you’re ready to explore this model for your practice (or as a patient), choose a provider who clearly outlines their virtual process, integrates remote monitoring, shows transparent pricing and maintains licensure and privacy compliance. When done right, functional medicine through telehealth isn’t just a workaround for geography—it’s a strategic evolution in how we care for health.

